Flat Feet Pain Problems & Reconstruction Surgery Melbourne
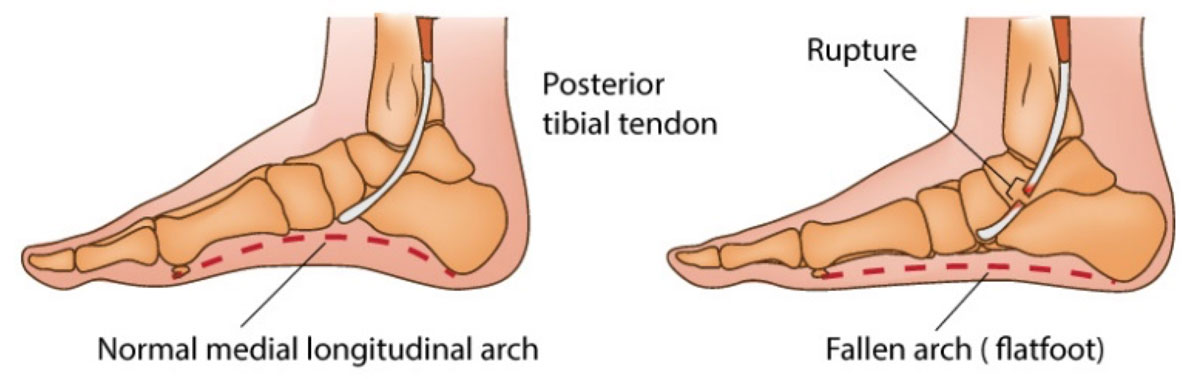
Flat Foot is the term used when the foot loses its normal arch, appearing flat against the ground. It is a complex process that involves problems with the tibialis posterior (TP) tendon, the spring ligament and the hindfoot joints.
The TP tendon is a large, important tendon that helps to hold up the arch of the foot and it can either tear or become damaged over many years. For this reason Flat Foot can also be called Posterior Tibial Tendon Dysfunction (PTTD) or Adult Acquired Flatfoot Deformity (AAFD).
The spring ligament is also important for maintaining the arch of the foot because it acts as a sling between the hindfoot and the midfoot. This, in conjunction with a torn or damaged TP, causes the joints to lose their normal alignment and thus the foot goes flat and can be very painful.
Symptoms
- Pain may commence along the arch of the foot and pain may develop on the outside of the foot.
- The foot flattens and turns outwards.
- Joints around the heel may become arthritic, leading to further stiffness and pain.
What Imaging is Needed?
You need to have an X-ray whilst standing to accurately assess the severity of Flat Foot.
You may also be asked to obtain a Magnetic Resonance Imaging (MRI) scan to assess the injury to the tendon.
NonSurgical Treatment
In many cases Flat Foot can be managed by non-surgical treatment. Physiotherapists or Podiatrists can discuss an exercise program to help retrain the muscles and Podiatrists can also provide you with an orthotic to provide arch support, which reduces demand on the tendon. Your Doctor can prescribe painkillers.
In many cases, Flat Foot can be managed by nonsurgical treatment.
When to consider having a discussion with your Surgeon for Flat Foot:
- When nonsurgical treatment such as exercises and insoles have been tried and you continue to have pain that is affecting your quality of life.
- Surgery is also considered if Flat Foot is stopping you from doing your usual, favourite and/or essential daily activities.
- Significant change in shape of foot that is affecting what shoes are worn.
Surgical Treatment
The aim of surgery is restoring the arch of the foot, which takes pain away and improves walking.There are two main options for surgical treatment of painful Flat Foot:
- Flat Foot reconstruction
- Hindfoot fusion
Hindfoot fusion is preferable if the joints under the ankle have become arthritic (painful and stiff). Please refer to the ankle arthritis page for details of this procedure.
Flat Foot reconstruction is complex and involves multiple operations around the foot. It usually involves repairing or strengthening theTP tendon by using another tendon called the Flexor Digitorum Longus (FDL), which normally has a role in bending the small joints in the lesser toes.This tendon is not missed for its original purpose.
In addition, the spring ligament is tightened during this operation and bony procedures (osteotomy with internal fixation), are used to reposition the heel bone to further support the arch of the foot. This is done by minimally invasive means.
Post-Operative Care for Flat Foot Reconstruction
- You must elevate the foot for 23 hours a day above the level of your heart for the first two weeks after surgery.
- You will have to non-weight-bear for a total of 6 weeks from the time of surgery.
- You will have a consultation with Mr Goldbloom 2 weeks after your surgery. Your slab will be changed to a boot and you are to remain non-weight-bearing with this for a further 4 weeks.
- Physiotherapy will be required post-operatively. It will be tailored to you and how well you are recovering.
Refer to the Foot and Ankle Surgery information sheet for further post-operative instructions.
Rehab Protocol for Flat Foot Reconstruction
| Week | Exercise | Boot/Crutches | Weight Bearing | Footwear | Returning to Function | Other |
|---|---|---|---|---|---|---|
| 0-2 | Boot exercises: Leg raises, buttock squeezes, quad squeezes, side lying hip abductions, deep breathing, toe wriggling | Hindfoot immobilised post-surgery. Crutch use. | Touch WB for 2 weeks (5kg) | Hindfoot immobilisation | Elevate above heart 23 hours per day | |
| 2-4 | Continue boot exercises. From week 3 complete active inversion and plantarflexion. | Thick sole Vacoped 30 degrees week 2 with crutches. Vacoped 20 degrees Week 3 with crutches. | Touch WB | Vacoped boot | At 3 weeks can remove boot at night. | Wound check with with Mr Goldbloom |
| 4-6 | Commence foot intrinsic and FHL isometrics with theraband. | Vacoped 10 degrees Week 4 with crutches. Vacoped 0 degrees Week 5 (wean off crutches). | 50% WB from week 4. Full WB from week 5. | Vacoped boot | At 4 weeks can 50% WB in boot. At 5 weeks can FWB in boot | |
| 6-8 | Commence active and passive dorsiflexion and eversion, progressing with the use of a theraband | Vacoped thin sole at 6 weeks. | FWB | Vacoped boot | Can swap to thin sole Vacoped | |
| 8-10 | Progress calf strengthening with seated and standing variations. Progress tib post, tib ant, peroneal loading. Add further proprioception and foot/ankle control exercises. Further mobility exercises if range of motion is limited. | Wean from boot from week 8-12. | FWB | Transition to normal shoes as wean from boot. | Wean from boot. Likely can return to driving if cleared and out of boot. Likely can resume further work depending on duties. | You may start to consider resuming light gym work |
| 10-12 | Start to incorporate more difficult balancing exercises with uneven/soft surfaces. Further strength and power progressions. Continue build walking load as tolerated. Start light jumping focusing on soft landing | nil | FWB | Normal shoes | ||
| 12+ | Include walking on different surfaces or longer walking. Begin return to running regime if favourable range of motion, strength (including plyometric exercise), power and proprioception has been achieved. | nil | FWB | Normal shoes | Begin further return to running and then sport. | It is important to note that while surgical healing is achieved it may take 6-9 months to regain your full strength. |
Download Flat Foot Rehabilitation Protocol
These programs have been developed by Mr Goldbloom in conjunction with Physiotherapists, Brodie Leonard-Shannon and Brendan Mason from Back in Motion, Aspendale Gardens.
Disclaimer: These tables are a guide only to base rehabilitation. Your Physiotherapist has a very important role in monitoring rehabilitation in case changes to fit your personal progress are required.
The information provided here is for general educational purposes only. Please contact Mr Goldbloom's rooms to discuss if surgery is appropriate for your situation.
